On this page you'll find basic overview instructions to re-enroll.
Select the section that best fits your needs.
On this page you'll find basic overview instructions to re-enroll.
Select the section that best fits your needs.
My name is Curtis Johnson, I wanted to shoot a short video introducing myself. It'll only take a couple minutes.
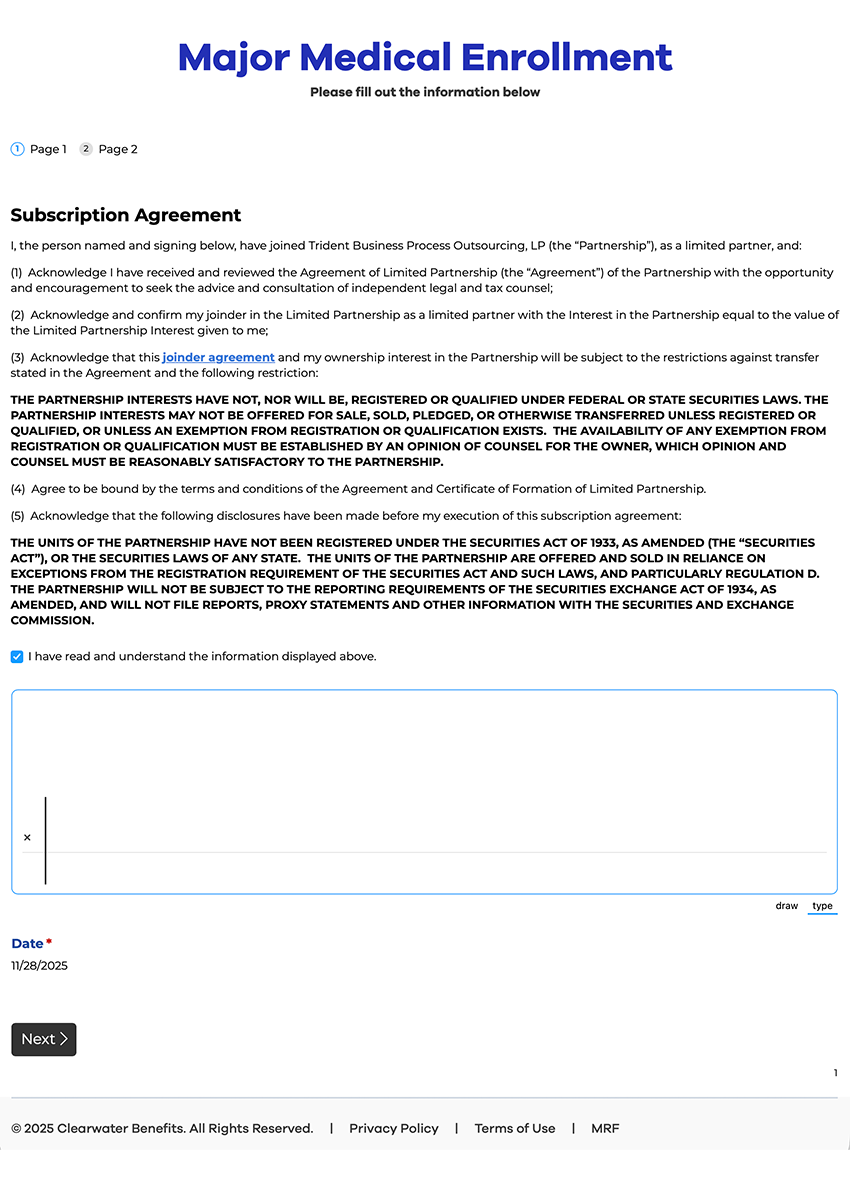
In the first section you are becoming part of the limited partnership. Its very important you read through the agreement.
Since you're re-enrolling, you should have already had this explained to you.
If you're not familiar with the LP, schedule a call and we can walk through it.
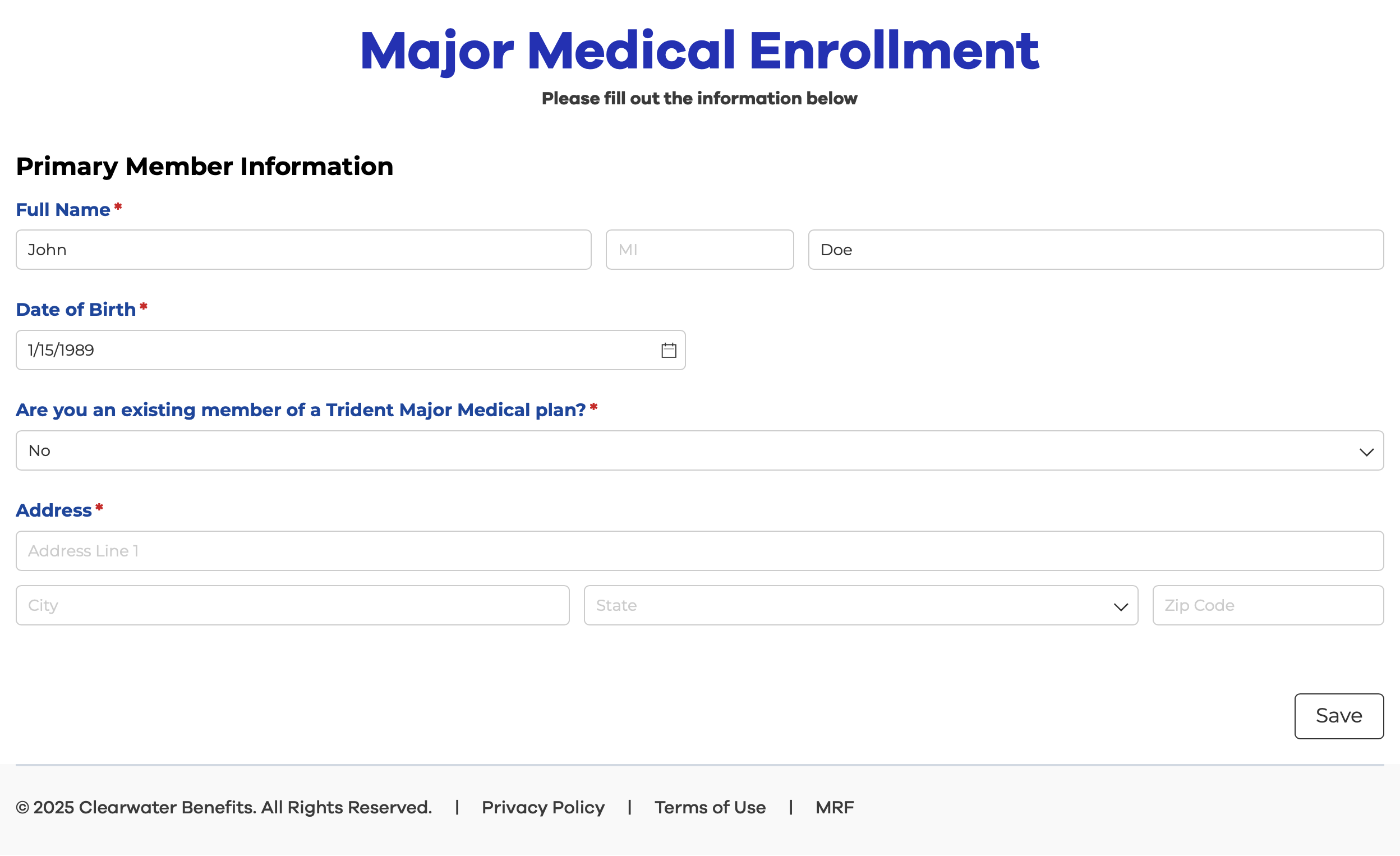
Please note in this section, you must include your existing Membership ID if you are a member of Trident already. If you're not, or have ClearShare, select "No" for "Are you an existing member of Trident Major Medical plan?"
In both cases you will see that your existing plans will end on December 31st 2025.
Again, select "Yes" if applicable.
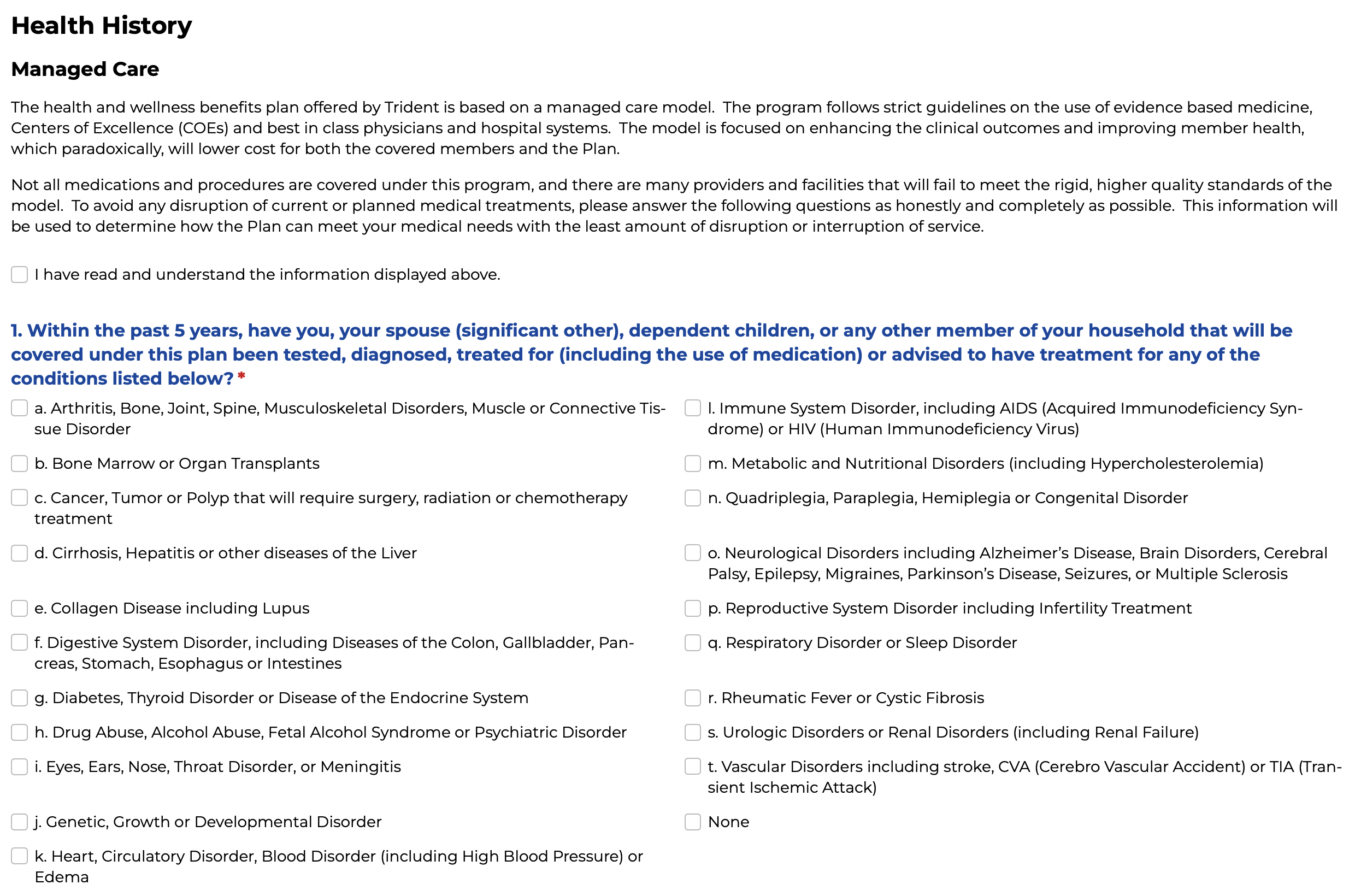
Please answer your health questions 100% honestly. Note that while health questions are asked in the application, the application clearly states pre-existing conditions are covered:
"I understand Trident’s health plan covers pre-existing conditions and based on my health status, I cannot be discriminated against in any way based on my health status. I understand that Trident may offer multiple plan design options with various types of coverage limitations, and it is ultimately my responsibility to thoroughly understand the coverage selection I choose."
Note, schedule a call with our team if you are treating a major or chronic diagnosis.
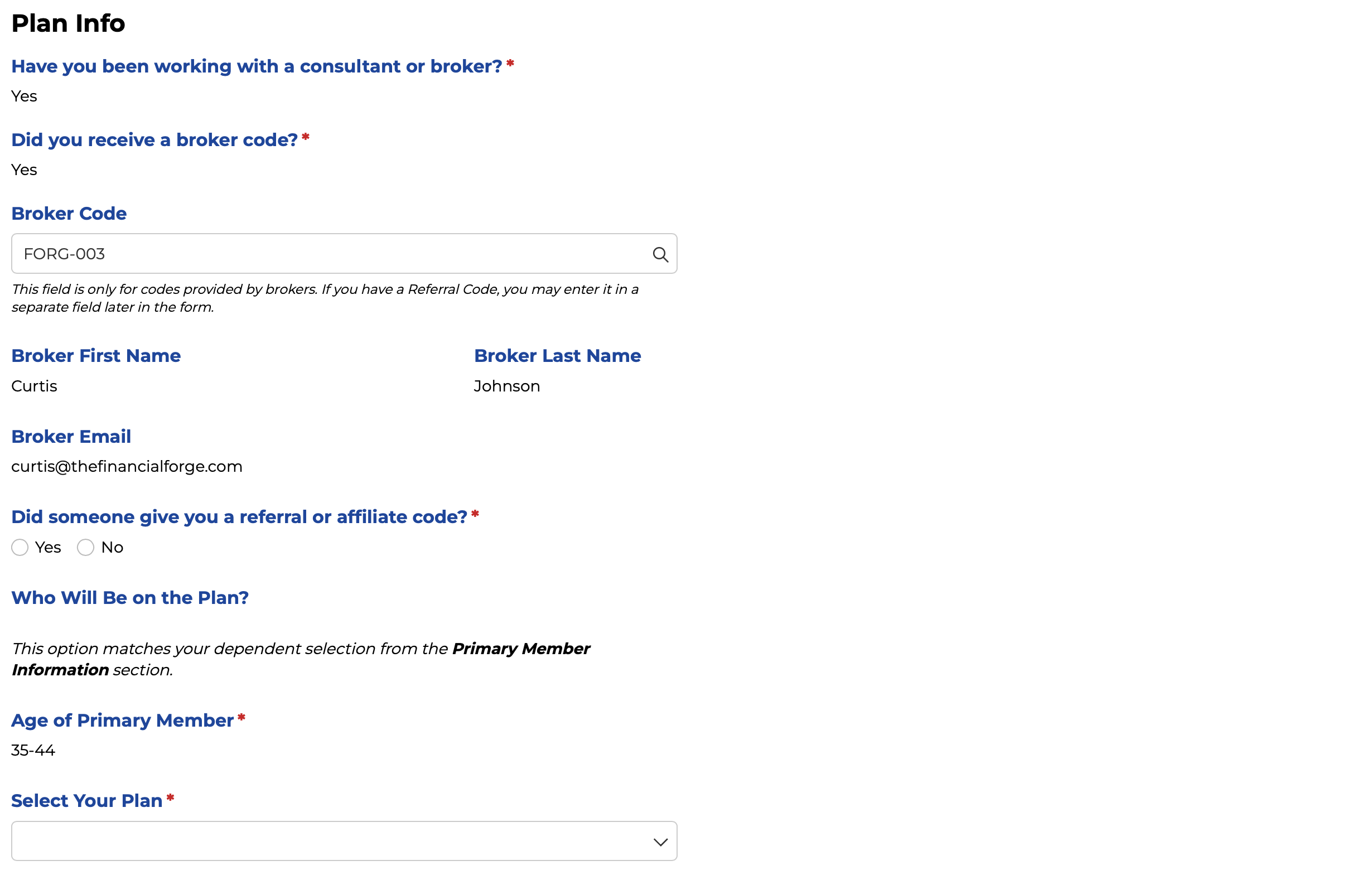
In this section you will confirm the plan and your broker.
You'll see a section called, "Broker Code" It should be prefilled with:
"FORG-003"
If not, fill that in. Where it asks about a "referral or affiliate code", select "No"
Under Select your Plan, fill out the plan that matches your selection from the quote.
While not all change is good, for the most part, the changes made to the 2026 Major Medical plans from Clearwater Benefits have shown to be a better fit for most of the clients we've already met with.
While many carriers across the nation are seeing between 20-40% increases, Clearwater's plans increased by 9 to 10% for 2026. You should already have your rates from your Broker.
You'll still have access to Tier 1 coverage. While not guaranteed, allowing Clearwater to find a provider for an imaging, surgery or procedure could result in your deductible being waived. (Tier 1 not available on the HSA 10,000 plan.)
Clearwater's 2026 MM plans have switched to the Prime Health Services Network. This changes increases the provider-count by over 200,000.
Explore the Provider NetworkMany MM plans now offer $0 generics and Name brands as long as they're on the formulary. There is only coverage for prescriptions on the plan's list of drugs - its formulary.
Search the FormularyLet's face it, while we understand these plans quite well, it's always smart to refer to the source. Please refer to Clearwater's Summary of Benefits and plan guides for details and clarification of any information provided here.
Developing a successful digital product is a complex process that requires choosing the right partner, applying innovative solutions, and following reliable processes.